Can DLL3-Targeted Immunotherapy Bring Hope to Patients with SCLC?
The approximately 30,000 Americans who will be diagnosed with small cell lung cancer this year face a poor prognosis.1 Scientists are hopeful that research based on targeting the delta-like ligand 3 (DLL3) protein may someday help these patients.2

Sponsored by Amgen
Precision medicine has driven a revolution in cancer treatment, providing new therapeutic approaches that are tailored to the unique biology of a patient’s tumors.3 But for patients fighting small cell lung cancer (SCLC) and the physicians treating them, it remains a race against time.4
While SCLC accounts for only about 15% of the 2.2 million patients diagnosed with lung cancer worldwide each year, it is one of the most aggressive and deadly solid tumor cancers.4-6 In fact, median survival is approximately 12 months or less following initial therapy.4 In the U.S., this year alone, approximately 35,000 people will be diagnosed with this devastating disease.1
SCLC: An aggressive disease with a poor prognosis and few treatment options
"SCLC continues to pose formidable challenges and remains a devastating disease for the majority of patients,” explains Taofeek K. Owonikoko, MD, PhD, Division Chief of Hematology-Oncology, University of Pittsburgh.
Because SCLC advances rapidly, roughly two-thirds of patients present with extensive-stage disease that has spread to distant parts of the body by the time of diagnosis.6 “If you look at the data, the 5-year relative survival for patients with extensive-stage disease SCLC is less than 7%, a number that hasn’t changed much over the past three decades,” says Dr. Owonikoko.1
There has been significant innovation in cancer immunotherapy but patients with SCLC who progress to later lines of therapy are in urgent need of additional treatment options.7
For decades, platinum-based chemotherapy has been a mainstay in SCLC treatment.4 While the disease is usually sensitive to initial treatment, the response is often short lived, followed by rapid and aggressive recurrences.8,9
“I think where the greatest unmet need resides is in second-line treatment and beyond,” says Dr. Owonikoko.10
Aiming to address the gap in SCLC patient outcomes, research scientists are investigating targeting a protein known as delta-like ligand 3, or DLL3, in patients with SCLC.2

DLL3: An exciting potential target for SCLC treatment
The DLL3 protein plays a key role in regulating Notch signaling, a pathway that is involved in embryonic development and neuroendocrine cell differentiation.6 In healthy cells, it is typically located intracellularly on membranes of the Golgi apparatus and cytoplasmic vesicles.11 In SCLC, DLL3 represents a an exciting potential therapeutic target as it is aberrantly expressed in SCLC in approximately 85-94% of patients, with minimal expression on normal cells.2,12,13 Moreover, aberrant DLL3 expression is consistent across all lines of treatment, which suggests the protein could play a role in therapeutic approaches for patients who have failed multiple lines of therapy and in earlier treatment lines.12
Dr. Owonikoko is excited about DLL3 as a new potential target. “DLL3 represents an exciting target for investigational T-cell engager therapy due to its aberrant expression in SCLC cases and a minimal expression on normal cells.”2,6
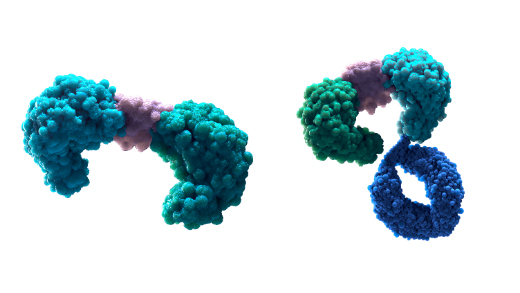
Targeting DLL3 through T-cell engagers
Cytotoxic T cells play a critical role in the adaptive immune system because they can differentiate between healthy and unhealthy cells.14 They can recognize malignant cells via TCR-MHC I binding, which can result in T-cell–mediated cancer cell lysis.15 However, cancer cells can avoid detection by downregulating MHC I and through an immunosuppressive tumor microenvironment for cancer cells.16
Accordingly, T-cell engagers are engineered with the goal of bypassing or outmaneuvering these avoidance mechanisms. T-cell engagers are designed to simultaneously bind to a tumor-associated antigen, in this case, DLL3, on the surface of cancer cells, and the CD3 protein on the T cell surface.16-18 This forms an immunological synapse between T cells and cancer cells, which can activate T cells without relying on normal TCR/MHC I recognition.16,19 Once activated, the T cells create perforin pores in the cancer cell membrane, allowing for the transfer of granzymes, which may induce cancer cell apoptosis, and proliferate locally, resulting in expansion of T cells to facilitate additional T-cell–dependent killing.19
The future of harnessing T-cell engagers to target DLL3 in SCLC
“Despite some of the progress we’ve made, SCLC remains an aggressive disease with a high unmet need,” remarked Dr. Owonikoko.4,10 “There is still need for additional and novel approaches that can improve outcomes for our patients.”6
In an era of personalized and targeted therapies, Amgen recognizes the significance of identifying and pursuing new targets, including exploring DLL3 in SCLC, and to harness the power of the immune system to offer new hope for patients with relapsed or refractory SCLC who currently have limited options.2,3
To learn more, visit www.DLL3possibilities.com.
Dr. Taofeek K. Owonikoko is a paid consultant for Amgen, Boehringer Ingelheim and Roche/Genentech; companies currently developing anti DLL3 therapies in SCLC.
©2023 Amgen Inc. All rights reserved.
References:
- American Cancer Society. Cancer Facts and Figures 2023. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2023/2023-cancer-facts-and-figures.pdf. Accessed September 17, 2023
- Paz-Ares L, et al. J Clin Oncol. 2023;41:2893-2903.
- Krzyszczyk P, et al. Technology (Singap World Sci). 2018;6(3-4):79–100.
- Oronsky B, et al. J Cancer. 2022;13:2945-2953.
- World Health Organization. Lung. 2020. https://gco.iarc.fr/today/data/factsheets/cancers/15-Lung-fact-sheet.pdf. Accessed September 17, 2023.
- Sabari JK, et al. Nat Rev Clin Oncol. 2017;14:549-561
- Qin A, et al. J Oncol Pract. 2018;14:369-370.
- Paz-Ares L, et al. Lancet. 2019;394:1929-1939.
- Horn L, et al. N Engl J Med. 2018;379:2220-2229.
- Coutinho AD, et al. Lung Cancer. 2019;127:53-58.
- Leonetti A, et al. Cell Oncol (Dordr). 2019;42:261-273
- Rojo F, et al. Lung Cancer. 2020;147:237-243.
- Saunders LR, et al. Sci Transl Med. 2015;7:302ra136.
- The Cleveland Clinic. Cytotoxic T-Cell. https://my.clevelandclinic.org/health/body/23547-cytotoxic-t-cells. Accessed September 17, 2023.
- Baeuerle PA, et al. Curr Opin Mol Ther. 2009;11:22-30.
- Yuraszeck T, et al. Clin Pharmacol Ther. 2017;101:634-645.
- Weidle UH, et al. Cancer Genomics Proteomics. 2013;10:1-18.
- Einsele H, et al. Cancer. 2020;126:3192-3201.
- Nagorsen D, et al. Exp Cell Res. 2011;317:1255-1260.